 Reaching menopause can wreak havoc on your skin. Skin
elasticity, acne, pore size, and pigmentation can all be affected by the
natural decline in reproductive hormones most women experience in their forties
and fifties, which results in the end of menstruation.
Reaching menopause can wreak havoc on your skin. Skin
elasticity, acne, pore size, and pigmentation can all be affected by the
natural decline in reproductive hormones most women experience in their forties
and fifties, which results in the end of menstruation.
But menopause and perimenopause do not have to be miserable
when it comes to skin woes. There is no denying that skin changes during
menopause can be both uncomfortable and distressing, so read on for insight
into what these changes might be, why they happen, and potential treatments
available to you.
Menopause equals low collagen
I often see patients complaining of jowls, slack skin, and wrinkles when perimenopausal or menopausal. During this time, the production of collagen, elastin, and hyaluronic acid exponentially decreases, and skin becomes thinner and drier. Research shows women’s skin loses about 30% of its collagen during the first five years of menopause, followed by a further 2% of collagen every year for the next 20 years.
The structural components of the dermis decrease, fat and bone are reabsorbed from the mid-central face, muscles relax, and fat deposits increase in the lower face. Clinically this translates in the shape of the face changing from an upright triangle to a downward triangle. Dynamic lines become more evident (crow’s feet, frown lines, and forehead lines), jowls appear, lines running from the tip of the nose to the corners of the mouth deepen. Smile and frown lines become visible all the time. Later, the tip of the nose dips, and you can see pouches under the eyes. But there are steps you can take to reduce these effects of collagen decline.
Most of these events are due to chronological ageing which is mainly genetic and difficult to prevent.
The skin also starts to show all the damage accumulated from sun exposure (mottled pigmentation, facial broken veins, skin coarseness, fine lines, and wrinkles) during the early decades.
What are the treatments for low collagen:
- Always protect the skin from the sun to reduce visible wrinkles, using a sun protection factor (SPF) of 30 or higher.
- Consider skincare products that contain retinol or peptides to increase the skin’s collagen level.
- Other options available are Botulinum Toxin (commonly known as Botox), dermal fillers and injectable anti-ageing treatment ‘Profhilo’, or potentially surgical options such as a face lift. A Dermatologist or Aesthetic Practitioner can explain these options to you and provide you with a consultation or referrals where needed.
Menopause and acne
Experts estimate that 25% of women aged 40 to 49 experience acne and, with many of those, it is related to menopause. In most cases, adult acne is caused by a hormonal imbalance impacting our skin’s natural defences. This is common when the body produces too much testosterone (male sex hormone) or increases sensitivity to normal levels of androgen within the skin.
These fluctuations can increase inflammation of the skin, cause a rise in oil (sebum) production, encourage the clogging of sebaceous glands, and stimulating the growth of the acne-causing bacteria Propionibacterium acnes.
 Perimenopausal acne develops in women for much of the same reason that it curses our skin in puberty. It certainly does not seem fair to battle wrinkles, menopause symptoms, and acne all at the same time. Dealing with all of this can also increase stress which is another acne trigger. Stress increases the levels of cortisol in the body, which increases breakouts through increased oil production.
Perimenopausal acne develops in women for much of the same reason that it curses our skin in puberty. It certainly does not seem fair to battle wrinkles, menopause symptoms, and acne all at the same time. Dealing with all of this can also increase stress which is another acne trigger. Stress increases the levels of cortisol in the body, which increases breakouts through increased oil production.
What treatments are there for menopausal acne:
Because a women’s skin is thinner and drier, treatments for teenage acne can be too harsh.
- Talk to your doctor or dermatologist about prescription medication.
- Hormone replacement therapy (HRT) is the most effective treatment for adult acne. However, you can still experience menopausal acne even if you are using HRT. This is because some HRTs use an influx of the hormone progestin to replace the oestrogen and progesterone your body loses. Introducing this hormone can cause your skin to breakout.
- Natural treatments are usually free of the side effects sometimes caused by prescription options.
- Speak to a Dermatologist or Aesthetic Practitioner about a treatment plan if you cannot get your acne under control.
What can I do at home to clear hormonal acne?
- Wash your face every morning and evening. Adding salicylic acid and/or glycolic acid into your routine can help to unclog pores.
- Apply no more than a pea sized amount of acne product. Applying too much can dry out the skin and cause irritation.
- Wear sunscreen every day and avoid tanning.
- Replace old, oil-based cosmetics with mineral-based ones.
- Think about making a few changes to your diet. Overdoing it on certain foods may lead to inflammation, so you might consider limiting dairy products, sugar, refined carbohydrates, and red meat.
- Kivu Anti-oxidant Mist is ideal for oily and combination skin. It helps to maintain essential moisture in the skin and its anti-oxidant properties assist in decreasing UV damage. This mist contains 70% Helix Aspersa secretion and bitter orange peel extract. It has astringent properties and is effective in healing acne blemishes.
- The combination of these two active ingredients has inflammatory, anti-microbial, anti-oxidant, and healing properties.
- Kivu Hydrating Elixir combines Helix Aspersa secretion with hyaluronic acid and has exceptional hydrating properties and a light texture. This product helps to moisturise dryness caused by acne-specific medical therapies (ie. retinoids).
Dry menopausal skin
One job of oestrogen is to stimulate the formation of the skin with smoothing collagen and oils. That is why when menopause approaches and oestrogen production diminish, skin can become dry and itchy. This is also exacerbated by the skin losing some ability to hold water. Pores often look larger when oil production drops, and hyaluronic acid levels also decrease, causing fine lines to become more visible.
Treatment for dry menopausal skin:
- Wash with a mild cleanser
- Apply moisturiser containing hyaluronic acid.
- Apply products containing Vitamin A derived molecules and glycolic acid to help the skin regenerate.
- Speak to a skincare specialist about treatment options such as Microdermabrasion.
- Kivu Anti-ageing face and eye cream is designed for mature skin, this unique 2-in-1 face and eye cream, uses the best active ingredients to improve skin hydration, skin brightness and elasticity. It will decrease the appearance of fine lines and blemishes as well as reducing puffiness under the eye. It combines Helix Aspersa secretion with peptides. It particularly has a high concentration of Acetyl Octapeptide-8 and Acetyl Tetrapeptide-5. Acetyl Octapeptide-8 has water binding properties hence it is able to hydrate, smooth and rejuvenate the skin, and Acetyl Tetrapeptide-5 reduces puffiness by changing the micro-circulation in the skin of the periorbital area, promoting lymphatic drainage.
Hyper-sensitive skin during menopause
 At around the age of 50, the PH level of our skin changes. With this change, skin becomes more sensitive and, women are more likely to develop rashes and easily irritated skin. Existing skin conditions such as eczema and rosacea could worsen, and you may need the help of an Aesthetic Practitioner or Dermatologist.
At around the age of 50, the PH level of our skin changes. With this change, skin becomes more sensitive and, women are more likely to develop rashes and easily irritated skin. Existing skin conditions such as eczema and rosacea could worsen, and you may need the help of an Aesthetic Practitioner or Dermatologist.
Treatment for hyper-sensitive skin:
- Use a fragrance-free moisturiser to reduce irritation.
- Use very mild cleansers.
- See a Dermatologist if your skin condition worsens.
- Kivu Firming Serum is effective for those who suffer from redness, rosacea or have sensitive skin. The product which combines the benefits of Helix Aspersa secretion and Witch Hazel and has a long-term soothing effect on the skin. Witch hazel is derived from the hamamelis virginiana plant and has the ability to soothe the skin and reduce inflammation.
Age spots and sun damage
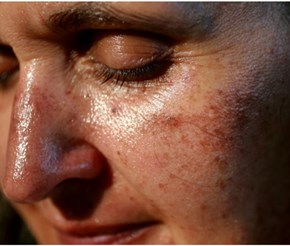 If you have spent ample time in the sun without skin protection, you will likely see the effects during menopause. Age spots (solar lentigo) can appear on all photo-exposed areas, but the face, hands, arms, legs, and chest are usually the areas of most concern.
If you have spent ample time in the sun without skin protection, you will likely see the effects during menopause. Age spots (solar lentigo) can appear on all photo-exposed areas, but the face, hands, arms, legs, and chest are usually the areas of most concern.
Another frequent condition that concerns menopausal women is the appearance of a condition due to chronic sun exposure called Poikiloderma of Civatte. It is a combination of thin skin, hypo or hyperpigmentation, and a net of dilated blood vessels that typically appears on the sides of the neck and characteristically doesn’t affect the skin under the chin and the top middle part of the neck. Many women think it is caused by the application of perfume, but this still hasn’t been fully demonstrated.
Actinic keratosis (precancerous lesions due to chronic sun exposure) starts manifesting. They are scaly, pink lesions that never heal.
Treatment and prevention of age spots:
- Apply a broad spectrum SPF30 (or higher) sunscreen every day before going outdoors. This can help fade age spots and prevent new spots from forming, which reduces your risk of developing skin cancer.
- Vitamin C and Vitamin A-derived molecules applied topically can help reduce pigmentation over time.
- Make an appointment to see a Dermatologist for skin cancer screening as the risk of skin cancer increases with age. The earlier you find skin cancer and pre–cancerous growths, the more treatable they are.
- Ask your Dermatologist to recommend treatment. Before you buy any products for age spots, see your Dermatologist for a skin examination.
Only really coming to mainstream awareness now, the effects of menopause on the skin are wide-ranging and can be tricky to handle. Now that you know what to expect, you are equipped to seek help or try our recommended at-home treatments to diminish these changes.
Whatever age you are, you do not have to live with dry, hyper-sensitive, inflamed skin, acne, or age spots.
The Menopause
 Natural menopause (when your periods stop) occurs at an average age of 51, but symptoms can start many years before. The medical definition of menopause is when your periods have stopped for a year. It occurs when ovaries stop producing eggs, which results in low levels of oestrogen, progesterone, and testosterone.
Natural menopause (when your periods stop) occurs at an average age of 51, but symptoms can start many years before. The medical definition of menopause is when your periods have stopped for a year. It occurs when ovaries stop producing eggs, which results in low levels of oestrogen, progesterone, and testosterone.
The impact of menopause is under-recognised, with more than 75% of women experiencing symptoms, a quarter having severe symptoms which may last seven years or more, and a third having long-lasting symptoms. A quarter of women have considered leaving or reducing their working hours due to symptoms.
What are the symptoms of menopause?
Symptoms of menopause are mainly due to fluctuating oestrogen and progesterone levels.
Periods start to become irregular. They can be more frequent or more spaced apart, heavier, or lighter. This disruption can go on for several years with or without other symptoms.
Most people are aware of hot flushes and poor sleep during menopause, but many other systems of the body are affected. Insomnia may happen due to night sweats or without them and, it is often one of the earlier symptoms. Some ladies suffer from restless legs that also affect sleep. Many women suffer from poor concentration and memory loss, as well as the inability to think clearly, also known as "brain fog." Anxiety, irritability, palpitations, and low mood are common.
Some ladies have joint and muscle aches and pains (even with regular exercise, menopausal women lose 2% of their muscle mass without extra oestrogen).
Most women eventually suffer from vaginal dryness. This can cause itching and discomfort (especially during sex) and bladder irritability that can lead to frequent urine infections. Loss of libido is a huge problem.
Skin becomes dry, loses elasticity, and may be itchy. Hair becomes thinner, and less shiny and dry eyes are common.
Migraine sufferers often find they get worse around menopause, again due to the fluctuation in hormones.
What are the longer term problems associated with low oestrogen levels?
Osteoporosis is a medical condition associated with bone fractures with minimal trauma and happens to many women after menopause due to low oestrogen levels. It is responsible for the loss of height many women experience with age and the stooping posture or Dowager's Hump.
Heart disease also increases in women after menopause. Before this, the incidence of heart attacks and angina in women is significantly less than in men, but this increases after menopause, and heart disease is the leading cause of death in women.
Treatment options
Many lifestyle changes can reduce symptoms: hot flushes can be reduced by cutting down alcohol and caffeine, weight loss and exercise are encouraged, and stopping smoking is always beneficial.
Herbal remedies
Herbal remedies such as soya, red clover, black cohosh, and St John's Wort have been found to help anecdotally, although the scientific evidence for them is not great. They are also generally not advisable to use in women who have had breast cancer, as they can interact with prescribed medications.
Prescribed Medication
Non-hormonal methods for reducing hot flushes include a blood pressure tablet called Clonidine and antidepressants such as Sertraline, Citalopram, or Venlafaxine. Some ladies also have good symptom relief with anti-epileptic medication such as Gabapentin and Pregabalin, although side effects are common.
Hormone replacement therapy (HRT)
Both oestrogen, and progesterone if required, are the most effective treatment for symptom control and will also address long-term conditions due to low oestrogen. These include maintenance of bone density and a consequent reduction in osteoporosis and fractures, protection against heart disease and vascular dementia (if started within ten years of the last period). HRT also reduces insulin resistance, and as a result, Type 2 Diabetes; it reduces osteoarthritis and bowel cancer; it improves vaginal dryness and bladder irritability (reducing the need to pass urine frequently).
The two main risks with HRT are breast cancer and blood clots.
 The risk of breast cancer is increased with combined HRT (oestrogen and progestogen) but probably not by oestrogen alone. The increased risk is similar to that of smoking, taking the combined pill, or drinking two units of alcohol each day. It is much less than the risk of breast cancer due to being obese.
The risk of breast cancer is increased with combined HRT (oestrogen and progestogen) but probably not by oestrogen alone. The increased risk is similar to that of smoking, taking the combined pill, or drinking two units of alcohol each day. It is much less than the risk of breast cancer due to being obese.
There is evidence that although the risk of getting breast cancer rises, the chance of dying from breast cancer is no greater than for women not taking HRT.
The risk of clots is not increased by using transdermal oestrogen (either a gel, spray, or patch so the oestrogen is absorbed by the skin), but it is increased by oral oestrogen.
What are the side effects of HRT?
Generally, HRT is well-tolerated, but one of the more common side effects when starting is some irregular vaginal bleeding. Bleeding should settle within three months or so, and if it does not, you should discuss it with your doctor as further investigations may be necessary.
Some ladies experience breast tenderness, fluid retention and bloating, headaches, nausea, and there may be an increase in vaginal discharge.
Some also have progesterone intolerance, and symptoms of this are similar to those with premenstrual syndrome.
Side effects are managed by changing the dose or type of HRT, and invariably women can find a regime to suit them.
How to take HRT
If you still have a womb you will need to take oestrogen (for symptoms) and progestogen to protect your womb, as oestrogen on its own can thicken the lining of the womb and increase the risk of cancer of the womb.
If you are still having periods or are within a year of your last period, then you take what is known as sequential HRT that is oestrogen every day, and progestogen for 12 -14 days every month.
If your periods finished more than a year ago, then you take continuous HRT that is both oestrogen and progestogen every day. However, if you have had a hysterectomy, you only need to take oestrogen.
HRT does not act as a contraceptive, so it is important to remember a woman needs to use contraception for a year after her last period if she is over 50 when they stop or for two years if she is under 50. If unsure of the final period, then contraception is needed up to the age of 55. One of the best ways to address both contraceptive need and the progestogen component of HRT is to use the Mirena coil, a device inserted into the womb. You can also take certain contraceptive pills with HRT or use barrier methods.
What are the different types of HRT?
Oestrogen comes in a patch, gel, or spray form (transdermal) or tablets, and as mentioned previously, the transdermal methods are the safest long term and have the lowest side effects.
Usually, we use Oestradiol which is a body-identical oestrogen. Some ladies also benefit from adding vaginal oestrogen to improve dryness and bladder symptoms.
Progestogen is available as the Mirena coil or as Utrogestan capsules (a body identical micronised progesterone), taken orally or sometimes vaginally. Micronised progesterone is the safest form of progestogen. Evidence shows a lower risk of breast cancer than with other types of progestogen, and also a beneficial effect on cholesterol. Progestogen is also available as a tablet either on its own or combined with oestrogen and, also as a combined patch.
Some women benefit from the addition of testosterone. This has been proved to help with low libido and sexual satisfaction, and some women also feel more energetic and notice an improvement in brain fog and muscle strength. We would not usually start testosterone until women have been on a good dose of oestrogen for several months. Testosterone is not licensed for women in the United Kingdom however, it is widely used by menopause specialists and some GPs. Side effects include acne and increased body hair, but there is no evidence of any long-term harm.
Generally, blood tests need to be done before starting and to monitor treatment with testosterone.
We do not usually do routine blood tests to diagnose menopause unless a woman is under 45. However, we may do blood tests when monitoring response to treatment, particularly if symptoms are not being controlled.
It may take some time to find a regime to suit you, but usually, a woman's quality of life is significantly improved by taking HRT. HRT can be continued long term after discussion with your doctor to fully understand the individual risks and benefits and effects on quality of life.
The risk of osteoporosis increases by smoking, lack of weight-bearing exercise, excess alcohol, and having a family history of osteoporosis.
Article by Holly Mason of The Skin Investment Clinic with contributions from: Dr. Alex Standring (menopause and HRT) and Dr. Benedetta Brazzini (dermatology and aesthetics)
Contact holly@theskininvestmentclinic.com for further advice and consultations.