What are genital
warts?
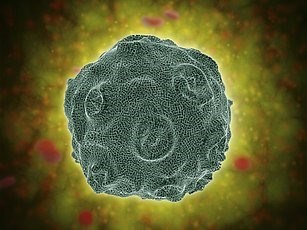 Genital warts is one of the most common sexually transmitted
infections – in fact, in England, the only STI that is more common is
chlamydia. Genital warts are caused by certain strains of the human papilloma
virus (HPV), a large group of viruses which mainly affect the skin. Other
strains of HPV are responsible for warts and verrucae found on the hands and
feet, plane warts which are usually found on the face, and changes in cells
which may lead to development of cancer – most commonly of the cervix. (1, 2,
3)
Genital warts is one of the most common sexually transmitted
infections – in fact, in England, the only STI that is more common is
chlamydia. Genital warts are caused by certain strains of the human papilloma
virus (HPV), a large group of viruses which mainly affect the skin. Other
strains of HPV are responsible for warts and verrucae found on the hands and
feet, plane warts which are usually found on the face, and changes in cells
which may lead to development of cancer – most commonly of the cervix. (1, 2,
3)
Genital warts can be unsightly, embarrassing and can cause
irritating symptoms, including itchiness, inflammation and disruption of flow
of urine, depending on the area affected. Fortunately, they are harmless, they
don’t lead to any serious conditions such as cancer, and they are not known to
affect fertility. There is no cure – once you have caught the virus, you will
have it for life. However, it is possible for your body to eventually clear the
warts in time, and there are also treatments available to help with this. (1, 4)
How do you catch
genital warts?
You don’t need to have penetrative sex to contract genital
warts – the skin of your groin area coming into contact with the skin of the
groin area of an infected person can be all it takes to pass the virus on.
Sharing sex toys can also lead to infection. Using condoms during sexual
activity is highly recommended to reduce the chance of transmission, but since
genital warts can affect the surrounding areas and upper thighs, infection can
still occur. However, don’t forget that condoms are a highly effective barrier
against other STIs, so unless you know for sure that you and your partner are
clear, you should be using them regardless! (4)
I think I might have
genital warts, what can I do?
If you think you might have genital warts, you can visit
your GP or a sexual health clinic for a diagnosis. They appear as painless
lumps on the vulva, penis, anus or surrounding areas, and can even be found on
the upper thighs. The warts can sometimes become itchy and inflamed, and if
warts are present inside the urethra (in men or women), the vagina or the anus,
this can lead to bleeding from these areas. Warts inside the urethra can also
cause urine to flow at an angle. On the other hand, you can carry the virus without
ever having shown any symptoms, or symptoms may develop years after exposure.
Despite this, you can still pass the virus on to others through sexual contact.
If you have a sexual partner who has genital warts, you should visit a sexual
health clinic, even if you don’t have any symptoms yourself. (4)
How are genital warts
treated?
Treatment for genital warts is prescription only. Don’t use
treatments for warts and verrucae, such as salicylic acid gel, found in
pharmacies and some shops to treat your genital warts – they are not designed for
this purpose and will irritate and damage the sensitive skin of your genital
area. (1)
Topical treatments (liquids and creams) which can be
prescribed to treat genital warts include podophyllotoxin,
a liquid that is applied to the warts with an applicator stick or as a cream. As the name
suggests, it is toxic to the warts and works by killing the cells. It is
applied in ‘cycles’ of three days followed by four treatment-free days. In most
cases, warts will disappear after four or five cycles. At Webmed Pharmacy we supply it under the brand name Warticon. It can be used for soft genital warts. (5)
Imiquimod (Aldara) is a
cream which is applied to larger warts three times a week and left for six to
ten hours before being washed off. It encourages your immune system to fight
off the virus that causes the warts. Warts should begin to clear up within a
few weeks. Aldara can be used for both hard and soft warts not only on the genitals but also those visible in the anal area. (5)
Trichloroacetic acid
(TCA) is applied to small, hard genital warts once weekly by a healthcare
professional at a genitourinary medicine (GUM) clinic. It breaks down proteins
in the cells of the warts to kill them. Unlike the other topical treatments, it
is safe to use in pregnancy. (5)
Genital warts can also be removed using physical ablation:
Cryotherapy
is a procedure during which warts are frozen using liquid nitrogen, which can
cause a sensation of burning. Once the procedure is finished, the skin can take
up to three weeks to heal.
Excision
is surgical removal of warts, often used for harder warts. Once the warts are
removed, the area is stitched together and should heal within three weeks.
Electrosurgery
involves applying a metal loop to a wart, then using an electric current
through the loop to burn the wart. Because this procedure can be so painful,
general aesthetic is occasionally used.
Laser
surgery can be used for hard-to-access warts, such as those in the urethra
or anus. A laser is used to burn the warts, and as with electrosurgery, this
may be performed under general anaesthetic. The area may be painful for up to
four weeks after the procedure. (5)
It is important to avoid sexual activity until the area has
fully healed. (5)
Treatment for genital warts is now available to buy from
Webmed Pharmacy. You’ll just need to answer a few questions
about your symptoms, health and any other conditions so that the doctor can
determine whether the treatment is right for you. If so, as with all of our
other tests and treatments, your medication will be posted securely to an
address of your choice the following day within a one hour time slot!
References
NHS inform. Genital warts: About genital warts
[cited 23 June 2019]. Available at: https://www.nhsinform.scot/illnesses-and-conditions/sexual-and-reproductive/genital-warts
Mayo Clinic. HPV infection: Overview [cited 23
June 2019]. Available at: https://www.mayoclinic.org/diseases-conditions/hpv-infection/symptoms-causes/syc-20351596
NHS. Warts and verrucas [cited 23 June 2019].
Available at: https://www.nhs.uk/conditions/warts-and-verrucas/
NHS. Genital warts [cited 23 June 2019].
Available at: https://www.nhs.uk/conditions/genital-warts/
NHS inform. Genital warts: Treating
genital warts [cited 23 June 2019]. Available at: https://www.nhsinform.scot/illnesses-and-conditions/sexual-and-reproductive/genital-warts#treating-genital-warts
Author
Gabby Gallaher MPharm
Medically reviewed by
Superintendent pharmacist Margaret Hudson
BSc(Hons) MRPharmS
2nd July 2019