Posted 30 August 2017
in Womens health
Polycystic ovary syndrome (PCOS) is a condition of which
there is still little awareness in society, despite it affecting up to one in five women. (1) Many of these
women remain undiagnosed due to simply not visiting their doctor because of
lack of knowledge of the condition and its symptoms. Some may have consulted
healthcare professionals, but have been misdiagnosed. Others may be reluctant
to discuss their symptoms due to the long standing societal issue of ‘women’s
problems’ not being taken seriously.
What is PCOS?
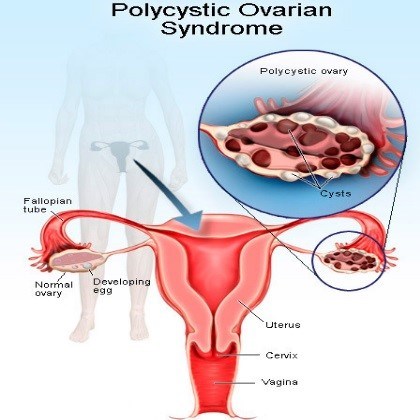
Women with PCOS often present with at least two of three
predominant symptoms: irregular periods,
excessive androgens (‘male hormones’) in the blood, and polycystic ovaries. The former two
usually manifest as identifiable symptoms - affected women may experience
erratic periods or none at all, and may exhibit male pattern hair growth
(thick, dark hair in unwanted areas including the face, chest, abdomen, back
and buttocks) as well as stubborn acne. (1, 2) The latter can only be confirmed
by having an ultrasound scan, and a positive result will show oversized ovaries
with a rugged, bumpy appearance which is caused by many fluid-filled sacs, or
follicles, inside the ovaries. When eggs are not released, follicles continue
to enlarge. (1, 3)
Other symptoms include tendency to gain weight, heavy
periods, tiredness, hair thinning and difficulty conceiving. (1)
What causes PCOS?
A concrete cause of PCOS has not been found, but it is
believed that hormone imbalance plays a major role. PCOS sufferers experience
resistance to the effects of insulin,
the hormone enabling the body to absorb glucose (sugar) after meals for energy
stores. Therefore, more insulin is produced to make up for this, which in turn
stimulates the ovaries to produce excessive amounts of the male hormones
responsible for PCOS symptoms. (1)
Persistent insulin resistance can also increase the risk of
type 2 diabetes later in life for those with PCOS. (1)
Is there a cure?
Unfortunately there is no cure for PCOS, but the symptoms
can often be controlled through diet and lifestyle changes and medication.
Being overweight can worsen insulin resistance, so
maintaining a healthy weight will help to ease symptoms. (1) Aim for 30 minutes
of moderate intensity exercise 5 days a week and a diet high in vegetables,
fruit, fibre and lean protein and lower in fat and sugar.
Various medicines can also be used to help alleviate PCOS
symptoms.
The combined
oral contraceptive pill reduces the release and effects of male hormones
and associated symptoms (excessive hair growth and acne) as well as regulating
periods.
Spironolactone
is another medicine that works against male hormones.
Metformin
can help combat insulin resistance, reducing symptoms and promoting weight loss
and fertility.
Clomifene is
used for women who are struggling to get pregnant. It helps the ovaries to
release eggs on a monthly basis. (1)
In a procedure known as laparoscopic ovarian drilling, the
ovarian follicles are treated with a laser or heat, stopping production of the
male hormones to improve symptoms and fertility. (1)
With a variety of options available to control the symptoms
of PCOS, and the opportunity to vastly increase awareness of the condition, the
prognosis should not be seen as bleak. If you are a woman experiencing some of
the symptoms listed above and think you may have PCOS, speak to your GP.
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 30/08/17
References
[1] National Health Service. Polycystic ovary syndrome [cited
25 August 2017]. Available from: http://www.nhs.uk/Conditions/Polycystic-ovarian-syndrome/Pages/Introduction.aspx
[2] PCOS UK. Polycystic ovaries and polycystic ovary
syndrome [cited 25 August 2017]. Available from: http://www.pcos-uk.org.uk/about-pcos.html
[3] PCOS Awareness Association. What is an
ovarian cyst? [cited 25 August 2017]. Available from:
http://www.pcosaa.org/what-is-an-ovarian-cyst