Posted 10 October 2017
Affecting as many as 20% of women and 7% of men, migraine is
a big problem in society. It can make sufferers’ lives a misery, with some left
bedridden for days as they wait for symptoms to pass and then to recover. The
upside is that there is a plethora of treatment options and lifestyle tips that
can help to reduce or even banish migraines for good! (1)
What is migraine?
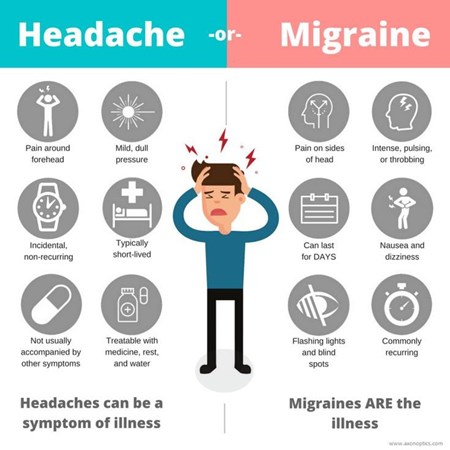
Migraine is a type of headache, usually experienced as a
throbbing sensation on one side of the head. This is often accompanied by nausea
(feeling sick) and sometimes vomiting (being sick). During a migraine, bright
light, loud sounds, or sudden movement of the head can make the pain
temporarily worse. They usually first appear when sufferers are young adults,
but may start earlier or later in life than this. (1) A single migraine attack
may last as long as three days.
Not all migraines are the same. Migraines with aura, also known as classic migraine, occur in
around one in three migraine sufferers. Before the throbbing headache starts, other
symptoms called aura appear, including visual disturbances (flashing lights,
patterns or blind spots in the field of vision), numbness that migrates from
the hand to the face, dizziness, slow speech, and less commonly, fainting. Migraines without aura, also known as
common migraine, comes on without any of the aforementioned aura. Less common
is migraine aura without headache,
also called silent migraine, which involves the occurrence of aura, but not
followed by a headache. (2)
What causes migraine?
It is believed that migraines occur due to temporary changes
in the brain, causing it to function abnormally. The root cause of these
changes has not been established, but it is known that in many sufferers, there
are particular ‘triggers’ that induce a migraine attack. Triggers differ from
person to person and may include sudden changes in temperature, stress, strong
emotions, low blood sugar, bright light or loud sounds, and sleep deprivation.
In some women, migraines occur at the start of their period, or a few days
before. This is thought to be caused by the drop in steroid hormones that
precedes a period, creating a withdrawal headache. Some people find that
certain foods and drinks bring on a migraine, such as alcohol, caffeine, cheese
and chocolate. However, it is thought that sufferers may experience cravings
for some of these products as part of the prodromal (pre-headache) stage of the
migraine, in which case consumption of said products would not be a trigger,
but a symptom. (3)
It can be useful for sufferers to keep a diary of what seems
to trigger their migraines, so that they can try to avoid these triggers where
possible in future. (3)
How is migraine
treated?
There are a number of medications available to treat
migraines, including:
Painkillers
such as paracetamol, ibuprofen, aspirin and co-codamol can be helpful,
especially if taken as early on in the attack as possible. This is because the
gut becomes sluggish during a migraine, meaning tablets or capsules will take
longer to dissolve and be absorbed. If painkillers cannot be taken as soon as
possible, an effervescent tablet form which is dissolved in water before taking
is the best option.
Triptans such
as sumatriptan and zolmitriptan are the next step if
painkillers are not enough to ease migraine. They work by undoing the temporary
changes in the brain that induce symptoms.
Anti-emetics
such as metoclopramide and domperidone are traditionally used to
relieve nausea and vomiting associated with migraine, but may relieve migraines
themselves, even if there is no nausea or vomiting present.
Combination
medicines combine painkillers with anti-emetics in one convenient tablet.
With painkillers and triptans, it is important not to use
them too frequently as this can cause medication overuse headache. If you find
that you are needing to use these medicines frequently, see your GP for an
alternative or preventative medication. (4)
How is migraine
prevented?
As well as avoiding triggers, medication can be taken to
prevent migraine attacks from developing in the first place.
Topiramate, originally
used as an antiepileptic, can be taken once a day as a tablet to prevent
migraines.
Propranolol
is a type of medicine known as a beta-blocker, originally used for high blood
pressure and angina, which has also been found to help prevent migraines. It is
available in tablet form and is taken daily in a single or divided dose.
Botulinum toxin
type A, also known as botox, is a toxin derived from the botulinum bacteria
which paralyses muscles. It is given in injection form to numerous parts of the
head and neck for migraine sufferers experiencing attacks on 8 or more days
each month and have had no success with other preventative medications.
For migraine related to the onset of a menstrual
period, non-steroidal anti-inflammatory
drugs (NSAIDs) or triptans can
be taken from two days before the period begins to the end of the period to
prevent migraine. Alternatively, hormonal contraceptives may be used or
oestrogen patches or gels applied from three days before the beginning of the
period and stopped after a week.
Acupuncture can
be tried as a last resort. (5)
If you think you may be experiencing migraine, or you are
taking treatment but it is not working effectively, see your GP.
References
- National Health Service. Migraine [cited 29 September 2017]. Available from: http://www.nhs.uk/Conditions/Migraine/Pages/Introduction.aspx
- National Health Service. Migraine - Symptoms [cited 29 September 2017]. Available from: http://www.nhs.uk/conditions/migraine/Pages/symptoms.aspx
- National Health Service. Migraine - Causes [cited 30 September 2017]. Available from: http://www.nhs.uk/Conditions/Migraine/Pages/Causes.aspx
- National Health Service. Migraine - Treatment [cited 30 September 2017]. Available from: http://www.nhs.uk/Conditions/Migraine/Pages/Treatment.aspx
- National Health Service. Migraine - Prevention [cited 3 October 2017]. Available from: http://www.nhs.uk/Conditions/Migraine/Pages/Prevention.aspx
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 10/10/17
Posted in Men's Health, Womens health