Posted 10 November 2017
in Men's Health, Womens health
 Affecting as many as one million UK people annually,
norovirus is a scourge of the late autumn and winter months. It can occur all
year round, but its seasonal proliferation has led to it being labelled as the ‘winter
vomiting bug’. Fortunately, despite its unpleasantness, it is a condition that
can almost always be managed through self-care. (1, 2)
Affecting as many as one million UK people annually,
norovirus is a scourge of the late autumn and winter months. It can occur all
year round, but its seasonal proliferation has led to it being labelled as the ‘winter
vomiting bug’. Fortunately, despite its unpleasantness, it is a condition that
can almost always be managed through self-care. (1, 2)
What is norovirus?
Norovirus is a general term for a number of different
viruses that can be responsible for gastroenteritis (inflammation of the
stomach and intestines), the main symptoms of which are sudden onset nausea
(feeling sick), projectile vomiting (being sick with force) and diarrhoea.
Other symptoms can include mild fever, stomach ache and aching in the arms and
legs. Norovirus is highly contagious and often occurs in ‘outbreaks’ in which
several people in a particular area or institution, such as schools,
workplaces, care homes, hospitals, cruise ships or restaurants, are infected
around the same time. (1, 2)
What can I do if I
contract norovirus?
Norovirus is, on the whole, self-limiting. This means it
clears up of its own accord without treatment. It doesn’t usually take longer
than three days for the infection to run its course. Whilst you’re ill, these tips
should help you to deal with the symptoms and to make sure you stay
well-nourished and hydrated. (2)
Drink plenty of water as vomiting and diarrhoea
can cause dehydration. Juice or soup can be taken as well as water; however,
don’t give juice or fizzy drinks to children as it can make diarrhoea more
severe. Babies should be fed as normal, via breast or bottle.
Fever and body aches can be alleviated with
paracetamol.
Stay indoors and rest as much as possible to
allow your body to conserve the energy it needs to recover.
If you think you are able to eat, stick to plain
foods (such as bread, pasta, rice, potato).
Look out for dark urine and dry mouth – these
are signs of dehydration. Signs in babies and young children include a sunken
soft spot on the head (babies only), sunken eyes, reduced tear production,
urinating less frequently and, as with adults, dark urine and dry mouth. Rehydration
sachets to be mixed with water can be bought over the counter at pharmacies and
can be used at all ages.
Over the counter medication to help with nausea,
vomiting and diarrhoea, such as loperamide
and bismuth subsalicylate, can be
taken by adults. However, if you take any other medication, be sure to check
with the pharmacist or read the leaflet within the package to make sure these
products are safe to take alongside. (2)
Do I need to see the
GP?
Don’t go to your GP surgery if you have norovirus, as this
can assist its spread to other people. Additionally, as previously mentioned,
there is no treatment for norovirus. If you need advice, you can call NHS
Direct on 111 or speak to your GP over the phone. (2)
There are certain complications which can arise with
norovirus. If you experience any of the following, call your GP or 111 as soon
as possible:
Symptoms have not eased after three days
Blood in diarrhoea
Severe dehydration (dizziness, losing
consciousness, greatly reduced or no urination)
Your child has had at least six episodes of
diarrhoea or three episodes of vomiting in the last 24 hours
Your child isn’t as responsive as usual, has a
fever or a pallid appearance
You should also call for medical advice if you have a
serious health issue such as kidney disease, and you contract norovirus. (2)
Reducing the spread
of norovirus
Norovirus is highly contagious and it would be impossible to
completely stop the spread. Nevertheless, the following steps can help to
protect you and others around you during an outbreak.
Wash your hands regularly with soap and water.
This is especially important after using the toilet and before preparing or
eating food.
Regularly clean surfaces with a bleach-based
disinfectant.
Wash clothes, towels and bedding on a hot wash.
Don’t share towels.
Flush the toilet straight after an episode of
vomiting or diarrhoea and disinfect the area.
Wash fruit and veg before preparation and ensure
food is thoroughly cooked before eating.
- Don’t return to school or work or make hospital
visits before 48 hours have passed since your last symptom. (2)
References
NHS. Norovirus [cited 23rd April 2018]. Available from: https://www.nhs.uk/conditions/norovirus/
NHS Choices. Norovirus [cited 7 November 2017].
Available from: https://www.nhs.uk/conditions/norovirus/
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 10/11/17
Posted 1 November 2017
in Men's Health, Womens health
 With at least one million cases annually across the globe,
meningitis is a major concern, and its tendency to peak in the winter months
means now is the ideal time to review what we need to look out for. (1, 2)
With at least one million cases annually across the globe,
meningitis is a major concern, and its tendency to peak in the winter months
means now is the ideal time to review what we need to look out for. (1, 2)
What is meningitis?
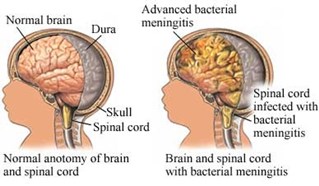
Meningitis means inflammation of the
meninges, which are the linings that shield the brain and spinal cord. (3) It
occurs most commonly in children under the age of 5, teenagers and those in
their early twenties, and people with weakened immune systems. (3, 4)
Viral meningitis
Viral meningitis is the most
common form, but is not usually serious. People infected generally recover with
no complications, although this may take some time, several months in some
cases. (1, 5) Enteroviruses, which are usually involved in milder illnesses
such as colds and upset stomachs, are the most common cause. (6)
Bacterial meningitis
Bacterial meningitis is the most
severe form. The cause is often particular bacteria that live harmlessly in the
nose or throat of healthy individuals that can be passed to others through
coughing, sneezing or close contact. Equally, if a person’s immune system
becomes weaker for whatever reason, they can also be at risk if any bacteria associated
with meningitis live in their body, as their defences may not be enough to stop
them from invading the meninges. (1, 4) Neisseria
meningitidis is the most common type of bacteria which causes meningitis,
followed by Streptococcus pneumoniae and Haemophilus influenzae Type B. (1)
Affected individuals can go from
feeling perfectly healthy to seriously ill within hours. Up to a quarter of
people who contract bacterial meningitis die as a result, many of whom will
have only started showing symptoms 24 hours earlier. (1) This is why it is
essential that we know the signs listed below and act immediately if we suspect
meningitis.
Fungal meningitis
Fungal meningitis is uncommon,
occurring mainly in those with weakened immune systems. It is caused by
breathing in fungal spores present in the air. It may be severe if it develops.
(1)
Other causes
Occasionally, meningitis may arise
as a result of injury, surgery on the brain, medication, cancer or parasitic
organisms. However, this is very rare. (1)
Signs and symptoms of meningitis
Recognising the following signs of
meningitis is crucial to enable treatment to be started as early as possible,
as the progression of the illness is so rapid. However, note that not all of
these symptoms may appear and there is no set order:
These symptoms call for an urgent
visit to A&E, or if you or the person concerned is too ill to get to
A&E, dial 999 immediately for an ambulance. It is a common misconception that
the main symptom of meningitis is the characteristic rash - this does not
always appear. If you are in any doubt, call 111 for NHS Direct. (3)
Vaccinations against meningitis
There are several vaccines
available that protect against different types of meningitis, the latest being
introduced in 2015 in the UK.
MenB
vaccine – this protects against the strain of Neisseria meningitidis known as MenB. This vaccine is given to
babies at the ages of 2 months, 4 months and 12 months. Since its introduction
in 2015, the number of babies contracting MenB has dropped significantly. (7)
MenC
vaccine – introduced in 1999, this offers protection against the MenC
strain of Neisseria meningitidis. It
is administered at the age of 12 months in combination with the Hib vaccine
and, since 2015, at 14 years as part of the MenACWY vaccine. It has almost
eliminated MenC meningitis in the UK. (7)
MenACWY
vaccine –protecting against the
MenA, MenC, MenW and MenY strains of Neisseria
meningitidis, this vaccine was introduced in 2015 to be routinely given to
14 year olds as a result of the rise of MenW cases in the UK since 2009. MenW
is a particularly dangerous strain, leading to death in a third of teenagers
who contract it. However, since its introduction, no teenagers who have
received the vaccine have fallen ill with any of the four strains it offers
protection against. (7, 8)
Pneumococcal
vaccine – this protects against a different type of meningitis-causing
bacteria, Streptococcus pneumoniae.It is given to babies at the ages of 2
months, 4 months and 12 months. (7)
Hib
vaccine – protecting against meningitis caused by Haemophilus influenzae Type B, this vaccine has cut cases
dramatically to almost none since it was introduced in 1992. It is administered
to babies at the ages of 2 months, 3 months, 4 months and finally 12 months.
(7)
MMR
vaccine – this vaccine offers immunity against the measles, mumps and
rubella viruses. These viruses can lead to viral meningitis in some cases. It
is given to babies at 12 months. (7)
For further information on
vaccines to protect against meningitis, click here.
References
Confederation of Meningitis Organisations. Types
of meningitis [cited 30 October 2017]. Available from: http://www.comomeningitis.org/facts-about-meningitis/types-of-meningitis/
Oxford Vaccine Group. Meningococcal disease
[cited 30 October 2017]. Available from: http://vk.ovg.ox.ac.uk/meningococcal-disease
NHS Choices. Meningitis [cited 30 October 2017].
Available from: https://www.nhs.uk/conditions/Meningitis/Pages/Introduction.aspx#outlook
Patient. Meningitis [cited 30 October 2017].
Available from: https://patient.info/health/meningitis-leaflet
Meningitis Research Foundation. What are
meningitis and septicaemia? [cited 30 October 2017]. Available from: https://www.meningitis.org/meningitis/what-is-meningitis
Meningitis Research Foundation. Viral meningitis
[cited 30 October 2017]. Available from: https://www.meningitis.org/meningitis/what-is-meningitis/viral-meningitis
Meningitis Research Foundation. Vaccine
information [cited 31 October 2017]. Available from: https://www.meningitis.org/meningitis/vaccine-information
Oxford Vaccine Group. MenACWY Vaccine [cited 31
October 2017]. Available from: http://vk.ovg.ox.ac.uk/menacwy-vaccine
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 01/11/17
Posted 26 October 2017
in Men's Health, Womens health
 Despite causing pain, itchiness and sometimes embarrassment,
warts and verrucae are not a serious condition and should clear up by
themselves for most people, although this may take years. Nevertheless, there
are treatments available if they are very bothersome or persistent. (1)
Despite causing pain, itchiness and sometimes embarrassment,
warts and verrucae are not a serious condition and should clear up by
themselves for most people, although this may take years. Nevertheless, there
are treatments available if they are very bothersome or persistent. (1)
What are warts and
verrucae?
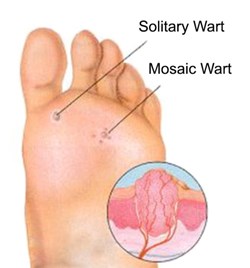
Warts and verrucae are small lumps of keratin (a protein
produced in the body which makes up hair and nails) that can form on any part
of the body, but usually the hands and feet. They are caused by particular
strains of the human papilloma virus (HPV). The term ‘wart’ is used for these
lumps when they occur anywhere apart from the soles of the feet, where they are
called verrucae (singular: verruca) or occasionally plantar warts. (1, 2)
The common wart is usually found on the fingers, but may
affect the palms, knuckles or even knees. It protrudes from the skin, is firm
to the touch and is characterised by a rough and rugged appearance. (1)
Verrucae are found on the soles of the feet. They differ
from common warts in that they are predominantly flat from the pressure put
upon them when walking, and contain small blood vessels which are visible as
black dots. (1, 2, 3)
Plane warts are flat warts found mainly on the face, the
backs of the hands, or the shins. They are yellow in appearance. They may occur
as a single wart or in hundreds! (3)
Mosaic warts are clusters of warts or verrucae. (1)
How are warts and
verrucae treated?
The most widely available and common treatment is salicylic acid, available in forms such
as gels, plasters and skin paints. These products can be purchased over the
counter at a pharmacy. Before applying the product, it is advised to soak the
wart or verruca in water for at least five minutes to soften the skin. Then,
carefully cover the healthy skin around the wart or verruca with a layer of
petroleum jelly, as salicylic acid may damage healthy skin. After doing this,
the product can be applied. This should be done on a daily basis. The wart or
verruca can be filed with an emery board weekly to remove dead skin, but ensure
that the emery board is thrown away after use and a new one used next time. (2)
Dimethyl ether
propane is available over the counter as a spray to freeze warts and
verrucae. However, it is not as effective as using salicylic acid products. (2)
If the wart or verruca persists despite use of these
products, visit your GP who may consider treatment with liquid nitrogen. This is applied directly to the wart or verruca
and works to freeze it off. It will need to be done numerous times to
completely clear the wart or verruca up. Unfortunately, this does not always
give the desired results, in which case your GP may refer you to a
dermatologist who may look into minor surgery and other treatment options. (2)
Other reasons you will need to see your GP for warts or
verrucae include:
facial warts, which should not be treated over
the counter, as the skin on the face is very delicate and can become damaged or
scarred easily
genital warts, which are caused by different
strains of HPV to those associated with common warts and verrucae, and should
be dealt with by your GP or a sexual health clinic
recurring warts
very big or painful warts
warts that bleed or change in appearance
diabetics
pregnant women
poor circulation in the hands and feet (2)
Protecting yourself
and others from warts and verrucae
Although warts and verrucae are very contagious, there are
steps we can take to reduce the spread. Touching warts and verrucae should be
avoided, and if touched, hands should be washed as soon as possible. In
communal places such as swimming baths and changing rooms, you should cover any
verrucae you have with a verruca sock or waterproof plaster. Do not share
footwear or towels with anyone else, and ensure you keep your feet and hands
clean and dry, including a fresh pair of socks daily. (2)
If you find a lump on your skin and are in any doubt as to
what it is or you are at all concerned, your local pharmacist is there to help.
References
National Health Service. Warts and verrucas
[cited 8th September 2017]. Available from: https://www.nhs.uk/conditions/warts-and-verrucas/
NHS Choices. Warts and verrucas [cited 24 October
2017]. Available from: https://www.nhs.uk/Conditions/Warts/Pages/Introduction.aspx
Bupa. Warts and verrucas [cited 23 October
2017]. Available from: https://www.bupa.co.uk/health-information/directory/w/warts-and-verrucas
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 26/10/17
Posted 19 October 2017
in Men's Health, Womens health
There are a number of conditions that can cause red eyes,
with conjunctivitis being a common one. Other symptoms include itching,
watering and sometimes stickiness of the eyelashes. The good thing is that in
most cases, it can be controlled without the input of your GP! (1)
What is
conjunctivitis?
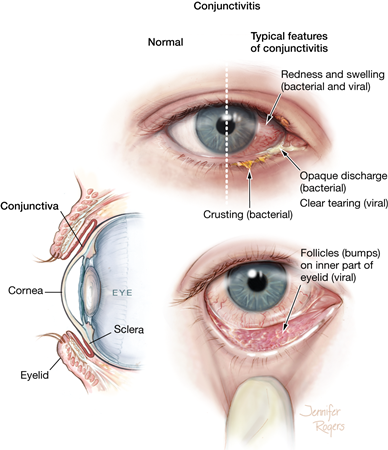
Conjunctivitis means inflammation of the conjunctiva, which
is a thin lining on the front of the eye. It can affect one or both eyes. (2)
What is the cause?
There is more than one cause of conjunctivitis, each of
which usually yields different symptoms.
Infective
conjunctivitis is caused by bacteria or a virus. As the name suggests, it
can be caught from and passed on to other people.
Bacterial conjunctivitis tends to produce a yellow pus
that leads to stickiness and crusting of the eyelashes. It is usually spread
when an infected person rubs their eyes, then touches a surface which is
subsequently touched by another person, who can contract the infection if they
then touch their own eyes.
Viral conjunctivitis is often associated with a gritty,
irritated sensation in the eye. It is passed to other people via coughing and
sneezing as well as physical contact, so is the more contagious form. (2,3)
Allergic
conjunctivitis is caused by allergens, usually pollen, dust mites or pet
dander, coming into contact with the eye and inducing a reaction. Symptoms
include itchy, red and watering eyes. It often appears with hayfever or
perennial rhinitis. (2,3)
Irritant
conjunctivitis is caused by foreign objects, such as a detached eyelash or
grit from the outdoors, getting trapped under the eyelid and rubbing against
the eye. It can also be caused by irritating substances such as shampoo or
chlorine-treated water found in swimming baths coming into contact with the
eyes. The eyes should return to normal shortly after the irritant is removed.
(2,3)
How is it treated?
Infective conjunctivitis is generally a self-limiting
condition, meaning it will probably clear up on its own, usually within a
couple of weeks. In the meantime, to ease the symptoms, you can bathe the
affected eye(s) in boiled and cooled water with the aid of cotton wool. If you
have bacterial conjunctivitis and bathing is not sufficient to control the
symptoms, visit your pharmacist who will assess your condition and sell you
antibiotic eye drops (chloramphenicol)
if they see fit. (1,2)
Allergic conjunctivitis can be managed with antihistamines,
either in eye drop form (sodium
cromoglicate) or taken by mouth in tablet or liquid form (such as chlorphenamine or loratadine). Avoiding contact with the allergen is also
recommended, which may involve regular thorough cleaning of your home to
minimise dust, or keeping windows closed where possible when the pollen count
is high. (2)
When to see your GP
Despite most conjunctivitis cases being easily managed
through self care or the pharmacy, there are instances where you will need to
visit your GP. Pain in the eye, changes in vision, sensitivity to light or
intensely red eyes all warrant an urgent GP appointment. Additionally, if you
have a child under the age of two years, you will need to take them to their
GP. (2)
Reducing the spread
of infective conjunctivitis
If you are suffering with bacterial or viral conjunctivitis,
be sure to wash your hands frequently and avoid touching your eyes. Do not
share pillows or towels.
You should be fine to go to work or school unless your
symptoms are severe and you don’t feel well enough to attend. However, if your
job involves close contact with people, or use of shared phones or computers,
it is advised that you stay at home until your symptoms have resolved, as the
infection may be more easily spread. (2)
References
- National Health Service. Chloramphenicol [cited 6 December 2018]. Available from: https://www.nhs.uk/medicines/chloramphenicol/
- NHS Choices. Conjunctivitis [cited 16 October 2017]. Available from: http://www.nhs.uk/conditions/Conjunctivitis-infective/Pages/Introduction.aspx?nobeta=true
- Optrex. What you need to know about conjunctivitis [cited 16 October 2017]. Available from: http://www.optrex.co.uk/eye-conditions/conjunctivitis/
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 19/10/17
Posted 13 October 2017
in Men's Health, Womens health
 It’s that time of year again – the weather’s getting colder,
the nights are drawing in and of course, the pesky common cold seems to be
everywhere!
It’s that time of year again – the weather’s getting colder,
the nights are drawing in and of course, the pesky common cold seems to be
everywhere!
Many people think that the terms ‘cold’ and ‘flu’ are interchangeable,
or that the flu is just a bad cold. It’s not surprising given that both share
certain symptoms and tend to appear at the same time of year. However,
different viruses are responsible for the common cold versus the flu, and the
latter can end up being more serious for particular groups of people. (1)
What are the
differences between cold and flu?
The common cold can be caused by a number of different
viruses, including the rhinovirus and the coronavirus. Flu (short for
influenza) is caused by influenza viruses. Despite the many similarities, there
are some differences in symptoms and onset time that may help you to determine
whether you are suffering from a cold or the flu. Firstly, colds tend to creep
up on you gradually over a couple of days, whereas the flu will make a person
feel unwell very quickly. Additionally, a blocked, runny nose and sore throat
is more likely to be associated with a cold, and bodily aches and pains occur
more commonly with the flu. People can feel very unwell during a bout of the
flu, often so much that they are bedridden. Conversely, a person will usually
feel well enough to go to work and get on with their everyday activities whilst
they have a cold. (1)
Will I need to see my
GP?
For most people, a cold or the flu will clear up on its own
within a couple of weeks and no trip to the GP will be needed. Resting
(especially for flu), drinking plenty of water and taking painkillers such as
paracetamol to ease pain and fever should help to alleviate symptoms until you
recover. However, there are certain groups of people who are more likely to
suffer complications including pneumonia and bronchitis whilst suffering with
the flu. If you fall into one of the following categories, see your GP if you
think you have the flu:
65 or older
diabetic
pregnant
serious heart problems
chest problems such as asthma
severe kidney or liver disease
weakened immune system
previous stroke or mini stroke
Your GP may consider prescribing oseltamivir or zanamivir,
which are antiviral medicines. (1,2)
You can also receive a free flu jab if you are in one of
these at risk groups. Care home residents and carers are also entitled. Speak
to your GP or pharmacist to book an appointment. (3)
Please don’t beg your GP for antibiotics! Antibiotics are
used to treat bacterial infections, whereas colds and flu are viral infections,
so they won’t help to ease your symptoms. Furthermore, overusing antibiotics
contributes to antibiotic resistance, which means if we are not careful with
the antibiotics we have today, they may become useless against the bacteria
they are supposed to target, making bacterial infections untreatable in future.
Reducing the spread
of colds and flu
When we have a cold or the flu, droplets containing the
virus are released into our surroundings when we cough or sneeze. These
droplets can become airborne and therefore can be breathed in by other people,
infecting them. Droplets may also settle on surfaces, and the virus can infect
others when they touch the surfaces, then touch their nose, mouth or eyes. We
can reduce the spread of these droplets by coughing or sneezing into a tissue,
then throwing the tissue away and washing our hands. Hands should not be used
to cover the nose and mouth when coughing or sneezing as this allows for transfer
of the virus to commonly touched surfaces such as door handles, keyboards, banisters
and even via a handshake! Surfaces should also be cleaned regularly. (1)
Getting a flu jab, particularly if you’re in an at risk
group, will not only protect yourself, but will also help to protect other
people you come into contact with. (1)
For any more information, speak to your local pharmacist or
read more here.
References
National Health Service. Cold or flu? [cited 10
October 2017]. Available from: http://www.nhs.uk/Livewell/coldsandflu/Pages/Isitacoldorflu.aspx
- National Health Service. Flu – Treatment [cited
10 October 2017]. Available from: http://www.nhs.uk/Conditions/Flu/Pages/Treatment.aspx
- National Health Service. Who should have the flu
jab? [cited 10 October 2017]. Available from: http://www.nhs.uk/Conditions/vaccinations/Pages/who-should-have-flu-vaccine.aspx
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 13/10/17
Posted 10 October 2017
in Men's Health, Womens health
Affecting as many as 20% of women and 7% of men, migraine is
a big problem in society. It can make sufferers’ lives a misery, with some left
bedridden for days as they wait for symptoms to pass and then to recover. The
upside is that there is a plethora of treatment options and lifestyle tips that
can help to reduce or even banish migraines for good! (1)
What is migraine?
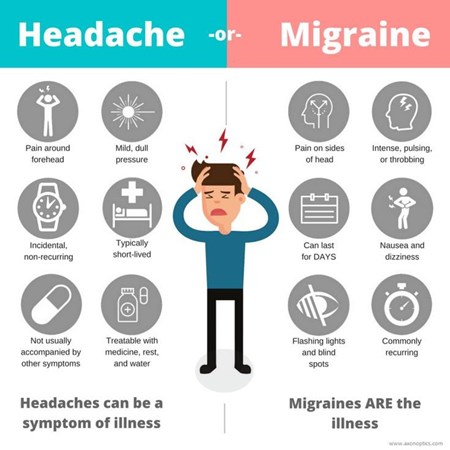
Migraine is a type of headache, usually experienced as a
throbbing sensation on one side of the head. This is often accompanied by nausea
(feeling sick) and sometimes vomiting (being sick). During a migraine, bright
light, loud sounds, or sudden movement of the head can make the pain
temporarily worse. They usually first appear when sufferers are young adults,
but may start earlier or later in life than this. (1) A single migraine attack
may last as long as three days.
Not all migraines are the same. Migraines with aura, also known as classic migraine, occur in
around one in three migraine sufferers. Before the throbbing headache starts, other
symptoms called aura appear, including visual disturbances (flashing lights,
patterns or blind spots in the field of vision), numbness that migrates from
the hand to the face, dizziness, slow speech, and less commonly, fainting. Migraines without aura, also known as
common migraine, comes on without any of the aforementioned aura. Less common
is migraine aura without headache,
also called silent migraine, which involves the occurrence of aura, but not
followed by a headache. (2)
What causes migraine?
It is believed that migraines occur due to temporary changes
in the brain, causing it to function abnormally. The root cause of these
changes has not been established, but it is known that in many sufferers, there
are particular ‘triggers’ that induce a migraine attack. Triggers differ from
person to person and may include sudden changes in temperature, stress, strong
emotions, low blood sugar, bright light or loud sounds, and sleep deprivation.
In some women, migraines occur at the start of their period, or a few days
before. This is thought to be caused by the drop in steroid hormones that
precedes a period, creating a withdrawal headache. Some people find that
certain foods and drinks bring on a migraine, such as alcohol, caffeine, cheese
and chocolate. However, it is thought that sufferers may experience cravings
for some of these products as part of the prodromal (pre-headache) stage of the
migraine, in which case consumption of said products would not be a trigger,
but a symptom. (3)
It can be useful for sufferers to keep a diary of what seems
to trigger their migraines, so that they can try to avoid these triggers where
possible in future. (3)
How is migraine
treated?
There are a number of medications available to treat
migraines, including:
Painkillers
such as paracetamol, ibuprofen, aspirin and co-codamol can be helpful,
especially if taken as early on in the attack as possible. This is because the
gut becomes sluggish during a migraine, meaning tablets or capsules will take
longer to dissolve and be absorbed. If painkillers cannot be taken as soon as
possible, an effervescent tablet form which is dissolved in water before taking
is the best option.
Triptans such
as sumatriptan and zolmitriptan are the next step if
painkillers are not enough to ease migraine. They work by undoing the temporary
changes in the brain that induce symptoms.
Anti-emetics
such as metoclopramide and domperidone are traditionally used to
relieve nausea and vomiting associated with migraine, but may relieve migraines
themselves, even if there is no nausea or vomiting present.
Combination
medicines combine painkillers with anti-emetics in one convenient tablet.
With painkillers and triptans, it is important not to use
them too frequently as this can cause medication overuse headache. If you find
that you are needing to use these medicines frequently, see your GP for an
alternative or preventative medication. (4)
How is migraine
prevented?
As well as avoiding triggers, medication can be taken to
prevent migraine attacks from developing in the first place.
Topiramate, originally
used as an antiepileptic, can be taken once a day as a tablet to prevent
migraines.
Propranolol
is a type of medicine known as a beta-blocker, originally used for high blood
pressure and angina, which has also been found to help prevent migraines. It is
available in tablet form and is taken daily in a single or divided dose.
Botulinum toxin
type A, also known as botox, is a toxin derived from the botulinum bacteria
which paralyses muscles. It is given in injection form to numerous parts of the
head and neck for migraine sufferers experiencing attacks on 8 or more days
each month and have had no success with other preventative medications.
For migraine related to the onset of a menstrual
period, non-steroidal anti-inflammatory
drugs (NSAIDs) or triptans can
be taken from two days before the period begins to the end of the period to
prevent migraine. Alternatively, hormonal contraceptives may be used or
oestrogen patches or gels applied from three days before the beginning of the
period and stopped after a week.
Acupuncture can
be tried as a last resort. (5)
If you think you may be experiencing migraine, or you are
taking treatment but it is not working effectively, see your GP.
References
- National Health Service. Migraine [cited 29 September 2017]. Available from: http://www.nhs.uk/Conditions/Migraine/Pages/Introduction.aspx
- National Health Service. Migraine - Symptoms [cited 29 September 2017]. Available from: http://www.nhs.uk/conditions/migraine/Pages/symptoms.aspx
- National Health Service. Migraine - Causes [cited 30 September 2017]. Available from: http://www.nhs.uk/Conditions/Migraine/Pages/Causes.aspx
- National Health Service. Migraine - Treatment [cited 30 September 2017]. Available from: http://www.nhs.uk/Conditions/Migraine/Pages/Treatment.aspx
- National Health Service. Migraine - Prevention [cited 3 October 2017]. Available from: http://www.nhs.uk/Conditions/Migraine/Pages/Prevention.aspx
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 10/10/17
Posted 29 September 2017
in Men's Health, Sexual Health, Womens health
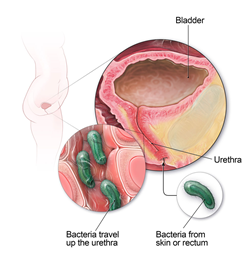 The
urinary tract is composed of the urethra, bladder, ureters and kidneys. The
blood is filtered through the kidneys to remove waste products and excess
water, forming urine. This then travels along the ureters to the bladder, where
it is stored until the person passes the urine out of their body via the
urethra.
The
urinary tract is composed of the urethra, bladder, ureters and kidneys. The
blood is filtered through the kidneys to remove waste products and excess
water, forming urine. This then travels along the ureters to the bladder, where
it is stored until the person passes the urine out of their body via the
urethra.
Urinary
tract infections (UTIs) can occur in any of these four areas. Depending on the
location, the infection may be labelled as urethritis (urethra), cystitis
(bladder), ureteritis (one or both ureters) or a kidney infection. (1)
Classic
symptoms include a frequent, urgent need to pass urine (often in small
amounts), a stinging or burning pain when passing urine, and lower abdominal
pain. However, the urine may also contain blood and may have an unpleasant
smell and/or a cloudy appearance. The person affected may feel generally
unwell, and elderly sufferers sometimes even experience confusion. (1)
What causes UTIs?
The most
common cause of a UTI is when faecal bacteria such as E. coli from the back passage get into the urethra. This happens
more frequently in women than men, because there is a shorter distance between
the openings of the urethra and back passage. Furthermore, the urethra itself
is shorter in women, meaning the bacteria don’t have as far to travel to reach
the bladder and higher portions of the urinary tract, leading to infection. (1)
The urinary tract is usually a sterile (bacteria free) environment, so it can
be quickly overwhelmed by invasive bacteria which have no competition for space
and nutrition.
Other
causes include conditions in which block part of the urinary tract, such as
kidney stones; an enlarged prostate in men, which can make complete emptying of
the bladder hard; a poorly functioning immune system, which increases a
person’s susceptibility to bacterial infections; using a catheter; and
pregnancy. (1)
How are UTIs treated?
For
women, sodium or potassium citrate
sachets are available that can be used at the first sign of a UTI. They help to
reduce the acidity of the urine, therefore easing symptoms while the body
fights the infection. One sachet is dissolved in a glass of water and taken
three times a day for two days. If the symptoms persist or recur after this
course, a GP appointment must be made as antibiotics may be needed to clear up
the infection.
Men,
pregnant women and children must be booked in to visit their GP upon the
development of any UTI symptoms. Anyone with lower back or side pain, a raised
temperature, chills, nausea, vomiting or diarrhoea related to a UTI should make
an emergency appointment with their GP, as the infection may have spread up the
urinary tract to the kidneys, which will need urgent treatment. (1)
Trimethoprim is the antibiotic of first choice for
simple UTIs affecting the urethra and/or bladder. Nitrofurantoin, cephalosporins
or norfloxacin can be used as an
alternative if the former is unsuitable, or the higher portions of the urinary
tract are affected. Courses of antibiotics must always be completed, even if
symptoms have ceased, otherwise the infection may not be fully treated and may
recur.
Paracetamol may also be taken for pain relief. (1)
Can UTIs be prevented?
There is
no failsafe way to prevent UTIs, but there are steps that can be taken to make
developing a UTI less likely. Always wipe from the front to the back after
using the toilet, to prevent transfer of faecal bacteria to the urinary tract.
Wear loose fitting, breathable underwear and try to use fragrance free body
washes and soaps in the intimate area. Drink plenty of water, try not to hold
in urine for too long and be sure to completely empty the bladder when you go
to the toilet. Also, pass urine as soon as possible after sex to flush out any bacteria
that have entered the urethra. (1)
If,
despite following these steps, you still suffer with recurrent UTIs, your
doctor may prescribe low dose antibiotics to help keep them at bay, or refer
you to a specialist for further investigation.
National
Health Service. Urinary tract infections (UTIs) [cited 24 September 2017].
Available from: https://www.nhs.uk/conditions/urinary-tract-infections-utis/
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 26/09/17
Posted 20 September 2017
in Men's Health, Womens health
 It was once a condition typically associated with rich,
overweight, port-drinking men and was grossly misunderstood. Nowadays, due to
changes in diet and lifestyle, gout is much more common within the general
population. Fortunately, we have the knowledge and means to manage it in an
effective way, and we don’t have to resort to trying the bizarre ‘remedies’ of
bygone times!
It was once a condition typically associated with rich,
overweight, port-drinking men and was grossly misunderstood. Nowadays, due to
changes in diet and lifestyle, gout is much more common within the general
population. Fortunately, we have the knowledge and means to manage it in an
effective way, and we don’t have to resort to trying the bizarre ‘remedies’ of
bygone times!
“Roast a fat old goose and stuff with chopped kittens, lard, incense,
wax and flour of rye. This must all be eaten, and the drippings applied to the
painful joints” - Lorenz Fries, 1518 (1)
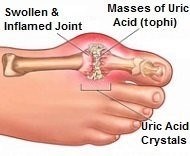
What is gout?
Gout is a form of arthritis (inflammation of the joints)
which affects up to one in fifty people in the UK, mostly men over 30 and
post-menopausal women. It typically occurs in the joints at or towards the
extremities of the body – the toes, fingers, ankles and wrists – but it can develop
in any joint. (2) In people affected by gout, the inflammation is caused by
build-up of crystals composed of sodiumurate within and around the joints.
(3) This leads to joints becoming painful, swollen and hot, with associated
tenderness. The skin surrounding the affected joints may also take on a shiny
appearance. Attacks of gout come on all of a sudden, with symptoms peaking
after a few hours. This persists for three to ten days, after which symptoms
subside. However, the gout will most likely recur at some point. (2)
What causes gout?
Uric acid is a metabolite
(breakdown product) of purines,
which are substances occurring naturally in the body. Purines are also found in
certain foods. The more purine-containing foods a person eats, the higher the
levels of uric acid in their blood. Excess uric acid can be filtered out of the
body via the kidneys, but if there is too much for the kidneys to deal with, it
can begin to be deposited at the joints as sodium urate crystals. Unbeknown to
them, a gout sufferer will have had these crystals developing in their joints
for years previous to their first attack. It is only when the hard crystals
build up so much that they invade the joint cavity and come into contact with
the soft tissue within the joint that symptoms develop. Over time, the crystals
may grow to such a size that they form tophi
that can disfigure the joint and be seen through the skin, occasionally even
erupting through the skin. (3)
Gout can run in families due to a genetic link, so if you
have a relative who suffers with gout you may be more likely to develop the
condition yourself. (2)
How can gout be
treated?
The aim of treatment during an attack of gout is to provide
symptomatic relief (reduce pain and inflammation).
Non-steroidal
anti-inflammatory drugs (NSAIDs) such as diclofenac, etoricoxib and
naproxen are the first port of call in treating an attack of gout. They
ease the inflammation and reduce pain. They should be taken as soon as symptoms
start to develop and should be continued throughout the attack and for the
following 48 hours once symptoms have subsided.
Colchicine
also reduces pain and swelling in affected joints and can be used as an
alternative to NSAIDs if they are unsuitable or have failed to provide relief.
Corticosteroids
also target inflammation and pain as a last resort for severe gout or if
other treatments are unsuitable. They may be administered in tablet form, or as
an injection to provide instant relief. (4)
How can gout be
prevented?
Both medication and lifestyle modifications can provide
protection from gout attacks.
Allopurinol
taken once daily is the first
choice preventative medication for gout. It works by decreasing uric acid
production in the body, thereby decreasing blood uric acid levels. However,
once started, it may trigger an attack of gout and attacks may continue for up
to two years before the preventative effects of allopurinol kick in.
Febuxostat
is an alternative once daily medication that also lowers uric acid
production. Like allopurinol it can cause an attack of gout at the beginning of
therapy.
Benzbromarone
and sulfinpyrazone can be
initiated by a specialist if other preventative medication has failed or is
unsuitable. (4)
Lifestyle changes
play an important role in preventing gout. Steer clear of foods containing high
levels of the purines which raise uric acid levels such as red meat, offal
(liver, kidneys, heart and sweetbreads), game, seafood, oily fish and meat or
yeast extracts (Marmite, Bovril and gravy). Cutting down on alcohol will help
as not only does alcohol stimulate the production of uric acid, it is also
metabolised to lactic acid which slows the filtration of uric acid out of the
body by the kidneys. Beer in particular should be avoided, as the fermentation
process used in its production results in a high purine content. Maintaining a
healthy weight will also help to keep attacks at bay, as being overweight
increases uric acid levels and puts more strain on some of the joints that can
be affected by gout. Additionally, drink plenty of water, as this can help your
kidneys to flush out the excess uric acid and to stop it turning into crystals.
(5)
Visit your GP if you think you may have gout, or if you do
have gout and your medication hasn’t eased your symptoms within two days.
References
Fries L (1518). Spiegel der Artzny. Strasbourg: Grüninger.
National Health Service. Gout [cited 18
September 2017]. Available from: http://www.nhs.uk/Conditions/Gout/Pages/Introduction.aspx
Arthritis Research UK. What causes gout? [cited
18 September 2017]. Available from: https://www.arthritisresearchuk.org/arthritis-information/conditions/gout/causes.aspx
National Health Service. Gout – Treatment [cited
18 September 2017]. Available from: http://www.nhs.uk/Conditions/Gout/Pages/Treatment.aspx
UK Gout Society. All about gout and diet. Available from: http://www.ukgoutsociety.org/docs/goutsociety-allaboutgoutanddiet-0113.pdf
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 20/09/17
Posted 14 September 2017
in Men's Health, Womens health
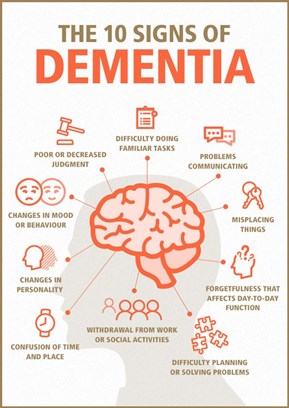 Dementia[1]
currently affects one in three people in the UK over the age of 65, with the
number set to inevitably rise as time progresses due to an ever aging
population. (1) So more than ever, it is important as a society to be aware of
the signs and how we can help sufferers, their families and friends in their
battle with the condition.
Dementia[1]
currently affects one in three people in the UK over the age of 65, with the
number set to inevitably rise as time progresses due to an ever aging
population. (1) So more than ever, it is important as a society to be aware of
the signs and how we can help sufferers, their families and friends in their
battle with the condition.
Dementia is far more than just ‘losing your marbles’. It is
a wide range of symptoms linked to deterioration in brain function, caused by
diseases of the brain. It not only affects memory, but language, perception of
the world around them, reaction times and judgement. A black mat on the floor
may appear to a dementia sufferer as a gaping hole, or a shiny surface may be
perceived as wet. Many aspects of life become more difficult, including
decision making, socialising, and thinking of the right words to use in
conversation. (1) People with dementia may become more isolated in turn, either
avoiding social situations or losing the company of friends and family who now
struggle to know how to act around them.
The causes and symptoms can vary depending on the type of
dementia.
Alzheimer’s Disease
This is the most common form of dementia. It is caused by
‘plaques’ of protein and ‘tangles’ of fibres forming in and around brain cells.
This results in damage to the nerve cells which relay signals in and out of the
brain, and also brain shrinkage. (2) One of the earliest symptoms is short term
memory loss – the affected person may struggle to remember the name of someone
they have recently met, or ask the same question over and over again. As more
areas of the brain become damaged, more symptoms will appear, such as a
reduction in organisational skills, confusion, reduced ability to problem solve
and mood changes. (3)
Vascular dementia
Vascular dementia occurs when the blood supply to the brain
is compromised, which leads to damage and death of brain cells. This can be a
result of a stroke or ‘mini’ strokes, or blood vessels within the brain
becoming narrowed or blocked. Symptoms include sluggish thoughts, waning
concentration, disorientation and balance problems. (4)
Dementia with Lewy
bodies
This form of dementia is caused by proteins accumulating
inside brain cells and forming deposits known as Lewy bodies. It is believed
that these deposits disrupt normal signalling between brain cells, leading to
difficulties with movement and processing visual information, sleep
disturbances, and alternating periods of alertness and confusion. (5)
Frontotemporal
dementia
A less common type of dementia, frontotemporal dementia
develops when protein deposits form specifically in the front and side sections
of the brain (frontal and temporal lobes). These areas are responsible for the
regulation of behaviour, speech and organisation. Therefore, associated symptoms
include behavioural changes – selfishness and lack of empathy, impulsiveness
and reduced motivation; slow and disordered speech, and reduced planning
abilities. (6)
Treatment and
management of dementia
Unfortunately, in most cases, dementia will only get worse
as time goes on. That’s why it is essential to get a diagnosis as early on as
possible and embark on the treatment that is available for some types of
dementia, which should help to slow the progression of the condition.
Acetylcholinesterase
inhibitors include donepezil,
galantamine and rivastigmine andare used for mild to moderate
Alzheimer’s Disease and dementia with Lewy bodies. They work by stopping the
breakdown of a chemical released by nerve cells called acetylcholine, which
helps the cells to communicate. These medicines may cause heart problems, so
ideally patients should be monitored via electrocardiogram (ECG). (7)
Memantine
is given in severe Alzheimer’s Disease, or when acetylcholinesterase
inhibitors are unsuitable or ineffective. It works by blocking glutamate, a
chemical that is released in large amounts in Alzheimer’s Disease sufferers and
worsens the damage to the brain. (8)
Antidepressants
can be used in dementia patients suffering with depression, which is often
linked to their struggle with dementia.
Antipsychotics
can be issued when aggression and other behavioural problems associated
with dementia may pose a threat to patients themselves or others. However, the
risks versus benefits should be thoroughly considered, as these medicines may
aggravate the remaining dementia symptoms.
Psychological
treatments may help to ease symptoms of dementia, but will not prevent
symptoms from getting worse. They comprise cognitive
stimulation therapy and reality
orientation therapy which are designed to help memory and state of mind, validation therapy which may help
sufferers to be less affected by perceived irrational thoughts, and behavioural therapy, designed to help
with problems such as aggression and depression. (7)
Helping people with
dementia
As dementia progresses, sufferers will likely become more
and more dependent on family, friends and other caregivers to look after them.
Still, there are numerous ways in which you can help someone with dementia keep
their mind active and experience pleasure in their day to day life.
Focus on helping the person to enjoy themselves. If they
have a hobby it can be very helpful for them to continue with this to keep
their mind active, as long as their condition allows. There might be a certain
song or photograph that helps them to revisit and talk about happy memories
from younger days, as long-term memory is usually much less affected than
short-term.
Assist the person where possible with everyday tasks they
now find more difficult, but be careful not to completely take over unless they
want you to, as this may reduce their sense of self-worth. Also, do not be
critical as this will probably discourage them from independent task handling
in future.
Some people with dementia may find that taking part in
creative activities or joining social groups really helps them to feel
accomplished and improve their quality of life.
This information is not exhaustive and much more support and
guidance can be found online. Visit www.dementiauk.org
or take six easy steps to become a Dementia Friend at www.dementiafriends.org.uk/register-digital-friend.
References
National Health Service. About dementia [cited 6
September 2017]. Available from: http://www.nhs.uk/Conditions/dementia-guide/Pages/about-dementia.aspx
National Health Service. Alzheimer’s disease –
Causes [cited 6 September 2017]. Available from:
http://www.nhs.uk/Conditions/Alzheimers-disease/Pages/Causes.aspx
National Health Service. Symptoms of dementia
[cited 6 September 2017]. Available from: http://www.nhs.uk/Conditions/dementia-guide/Pages/symptoms-of-dementia.aspx#alz
National Health Service. Vascular dementia
[cited 6 September 2017]. Available from: http://www.nhs.uk/Conditions/vascular-dementia/Pages/Introduction.aspx
National Health Service. Dementia with Lewy
bodies [cited 6 September 2017]. Available from: http://www.nhs.uk/Conditions/dementia-with-lewy-bodies/Pages/Introduction.aspx#causes
National Health Service. Frontotemporal dementia
[cited 6 September 2017]. Available from: http://www.nhs.uk/Conditions/frontotemporal-dementia/Pages/Introduction.aspx#treatment
National Health Service. How is dementia
treated? [cited 6 September 2017]. Available from: http://www.nhs.uk/Conditions/dementia-guide/Pages/dementia-treatment.aspx
Alzheimer’s Society. Drug treatments for
Alzheimer’s disease [cited 6 September 2017].
Available from: alzheimers.org.uk
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 14/09/17
Posted 4 September 2017
in Men's Health, Womens health
 “Pain so severe you
just want to die” –and yet
affecting approximately as many people in the UK as the widely known condition
multiple sclerosis (MS) (1), any mention
of cluster headaches will likely draw blank looks from most of the general
population. Given this, it’s hardly surprising that many sufferers feel alone in
their battle with the condition. (1)
“Pain so severe you
just want to die” –and yet
affecting approximately as many people in the UK as the widely known condition
multiple sclerosis (MS) (1), any mention
of cluster headaches will likely draw blank looks from most of the general
population. Given this, it’s hardly surprising that many sufferers feel alone in
their battle with the condition. (1)
What are cluster
headaches?
Cluster headaches (CH) differ vastly from a regular (tension)
headache. Attacks (individual headaches) come on very suddenly. During an
attack, sufferers experience a sharp, burning pain of excruciating intensity on
one side of the head. (2) In fact, women who have both given birth and have CH
have branded the latter as worse. (3) The pain is typically centred around the
eye, but may affect other parts of the head or neck. The side affected may
change between attacks, or less commonly, in the same attack. (4) Other
symptoms occurring alongside the headache can include a red, watering eye, a
congested or runny nostril, facial sweating, a droopy eyelid and a constricted
pupil. (2)
Unlike migraine sufferers who usually want to lie down and
rest during an attack, those with CH may pace around, rock their head or even
resort to banging their head against a wall due to the severity of the pain.
(2)
Attacks normally take place in bouts, or ‘clusters’, which
persist on average for a period of four to twelve weeks. Within a cluster,
attacks normally happen every day at the same time of day, and may occur
multiple times a day, beyond eight in some cases. (2)
The period in between clusters is known as remission, which
may last years before attacks return. However, many sufferers find they
experience clusters around the same time every year.
In some particularly unfortunate instances, sufferers
experience attacks on a chronic (ongoing) basis. This means they have
experienced attacks every day for a year or more with no remission period, or a
very short one. (3)
The excruciating pain of CH, along with the relentless
nature, has led to the condition being dubbed “suicide headache”. (5)
What is the cause?
As of yet, there is no known definitive cause of CH,
however, it is believed that malfunctioning of the hypothalamus, a part of the
brain responsible for many vital bodily functions and processes, is the most
likely basis. Additionally, CH is sometimes found to run in families,
indicating a genetic link. (6)
How is it treated?
There are treatments available both to stop an attack from
progressing and to prevent attacks from happening in the first place.
The following are abortive
medications, used to treat individual attacks:
Sumatriptan,
when used at the beginning of an attack, can bring the headache to a halt. It
comes in either injection form, which can be self-administered once or twice a
day, or as nasal spray if preferred.
Zolmitriptan
is a similar medicine to sumatriptan and is available in a nasal spray form.
Pure
oxygen can be breathed through a mask to provide relief from an attack.
Lignocaine
is an anaesthetic administered in nasal drop or spray form. It is usually
not sufficient to stop an attack completely, but can be helpful when used
alongside other medicines.
A gammacore
device is a handheld appliance that can be held to the neck to generate a
pulse which stimulates the vagal nerve, which is believed to play a role in CH.
This can stop an attack in its tracks. (2, 7)
The following medications are preventative:
Verapamil
is the most common medicine used to prevent attacks. It may cause heart
problems, so it is important to have regular electrocardiogram (ECG) tests
during treatment.
Local
anaesthetic injections to the back of the head, corticosteroids or lithium are
alternatives if verapamil is ineffective or unsuitable. (2)
It is thought that certain triggers can bring on attacks in
some people. The smell of pungent chemicals, such as perfume or petrol, has
been known to be a trigger. Also, avoidance of alcohol and smoking cessation is
recommended. (2)
If these symptoms sound all too familiar and you think you
may have cluster headaches, make an appointment with your GP as soon as you can.
They will rule out other causes and assess your condition. Once you have a
formal diagnosis, you should then be referred to a specialist who will discuss
a treatment plan with you and help you to regain control over your life! (2)
For further support and information, visit ouchuk.org.
References
OUCH UK. Organisation for the Understanding of
Cluster Headache [cited 3 September 2017]. Available from: https://ouchuk.org/
National Health Service. Cluster headaches
[cited 3 September 2017]. Available from: http://www.nhs.uk/conditions/cluster-headaches/Pages/Introduction.aspx
OUCH UK. What is Cluster Headache? [cited 3
September 2017]. Available from: https://ouchuk.org/what-is-cluster-headache
OUCH UK. Cluster Attack [cited 3 September
2017]. Available from: https://ouchuk.org/cluster-attack
Medscape (2015). Hope for 'Suicide Headache'.
[online] Available from: http://www.medscape.com/viewarticle/844217 [Accessed 3
Sep. 2017].
OUCH UK. Causes [cited 3 September 2017].
Available from: https://ouchuk.org/causes
OUCH UK. Abortive Medication [cited 3 September
2017]. Available from: https://ouchuk.org/abortive-medication
Author: Gabby Gallagher MPharm
Medically reviewed by: Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS 04/09/17