Posted 14 March 2019
 Parkinson’s disease affects one in every 500 people, with
symptoms beginning to show over the age of 50 in most cases, but for 5% of
people with the condition, symptoms will first appear before the age of 40. It
can have a devastating impact on a person’s quality of life, with movement,
balance, memory, mental health and sleep all having the potential to be
affected. Current treatment aims solely to ease symptoms and does not cure the
condition. But a recent trial of an innovative therapy has hinted at new hope
for those with Parkinson’s disease. (1, 2)
Parkinson’s disease affects one in every 500 people, with
symptoms beginning to show over the age of 50 in most cases, but for 5% of
people with the condition, symptoms will first appear before the age of 40. It
can have a devastating impact on a person’s quality of life, with movement,
balance, memory, mental health and sleep all having the potential to be
affected. Current treatment aims solely to ease symptoms and does not cure the
condition. But a recent trial of an innovative therapy has hinted at new hope
for those with Parkinson’s disease. (1, 2)
What is Parkinson’s
disease?
Parkinson’s disease is a neurodegenerative disease involving
damage and death of dopamine-releasing nerve cells in a region of the brain
known as the substantia nigra, which regulates body movements. Dopamine is a
neurotransmitter, which is a chemical which acts as a communicator between
nerve cells. Therefore, the diminution in dopamine levels in the brain caused
by the death of these cells reduces intercellular communication relating to
movement and leads to tremor, sluggishness and stiffness. Symptoms do not
usually show until only around a fifth of these nerve cells remain. (2, 3)
In addition to the primary movement symptoms, people with
Parkinson’s disease can also experience a deterioration in mental health,
difficulty keeping balance (and therefore greater risk of falling), insomnia,
reduced sense of smell and poor memory. (2)
What is the outcome
of the recent trial?
The results of a recent trial of a radical treatment for
Parkinson’s disease have been released. The treatment, known as glial cell
line-derived neurotrophic factor (GDNF), is an entirely new approach,
administered via a ‘port’ that is embedded in the side of the patient’s head.
This allows the drug to be delivered directly into the brain, where it then
acts on dopamine nerve endings. (1)
Before the trial, the 35 participants had surgery which
involved embedding four tubes into their brains. These tubes would be the route
of administration of the drug into the brain, with the outer end being attached
to the port where the drug would enter the tube. (1)
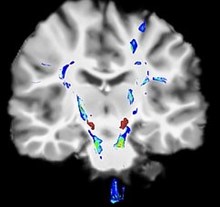
The trial lasted nine months, during which half of the
participants were administered with a dose of GDNF every month, with the other
half being administered a placebo infusion (containing no drug). For those
given the drug, brain scans after the trial suggested that the progression of
the disease had been significantly reversed. The average length of time since
diagnosis for the trial’s participants was eight years, but the post-trial
scans appeared to show features typical of brains just two years after
diagnosis. This implies that GDNF can revitalise dying nerve cells and restore
their function. (1)
However, it is too early to know whether GDNF will become a
routine treatment at this stage – more trials involving larger numbers of
participants, longer treatment courses and different doses will need to be
performed before its licensing is considered. The placebo effect will need to
be ruled out (this is when a participant being given a placebo experiences an
improvement in their condition or symptoms). (1)
Regardless, it is very exciting that new modes of drug
delivery such as this are being developed and tested. If successful, the
approach may even be used to develop treatments for other conditions affecting
the brain, including Alzheimer’s disease and brain tumours. (1)
References
Therrien A (2019). ‘Radical Parkinson’s
treatment tested in patients’, BBC News.
Available at: https://www.bbc.co.uk/news/health-47370498
NHS. Parkinson’s disease – Overview [cited 1
March 2019]. Available at: https://www.nhs.uk/conditions/parkinsons-disease/
NHS. Parkinson’s disease – Causes [cited 1 March
2019]. Available at: https://www.nhs.uk/conditions/parkinsons-disease/causes/
Author
Gabby Gallagher MPharm
Medically reviewed by
Superintendent pharmacist Margaret Hudson BSc(Hons)MRPharmS
14/03/19
Posted in Men's Health, Womens health